Food sensitivities: can I feel bad the minute I eat something?

Food sensitivities are becoming more and more predominant in today's society, a whooping 15 to 20% of the population of North America complains to being intolerant or sensitive to various foods. (7) This often comes with an array of additional symptoms that are labeled as functional gastrointestinal disorders or another term commonly used is IBS. In this blog we will define food sensitivities, explore why to develop over time and discuss a functional medicine approach to "desensitizing" a person from food sensitivities and eventually what to do to re-expand their diet. We will also explore why, in certain individuals, and exaggerated mast cell response can cause food sensitivities to present literally minutes after consuming the offending agent.
So what exactly are food sensitivities?
Broadly there are 3 main categories of reactions people have to food.
The first reaction is IgE mediated and this is where we find the typical food allergy and also anaphylaxis. This is a reaction that is immediate, within seconds to minutes and occasionally within a few hours and is triggered by foods such as peanuts or shellfish and it can be life threatening. The typical symptoms are an urticarial rash, sensation of swelling in the throat, difficulty breathing or wheezing, digestive symptoms such as diarrhea, dizziness or loss of consciousness, among others. This type of reaction, the anaphylaxis, is treated with an EpiPen followed by an emergency room visit.
The second type of reaction to food is also immune mediated but this time the IgG play a role. This reaction is typically considered delayed, typically within 2 to 5 days of exposure to the offending agent, this is the classical food sensitivity and it can present in numerous ways which we will detailed below.
The third type of reaction to food is a non immunological reaction, this is where we find lactose intolerance which is a reaction to lactose due to the deficiency of an enzyme called lactase which normally digest lactose, the manifestations of this reaction are typically abdominal cramps, bloating and diarrhea. Another example of a known immunological reaction is sensitivity to sulfites which are food additive contained in red wine, and susceptible individuals this presents with headaches or an urticarial rash.
Food sensitivities are a therefore an immune mediated reaction, through IgG production by the immune system to various foods that are contained in the diet of the affected individual.
But how exactly does the immune system decide to create antibodies against pieces of food? This is clearly an abnormal response by the immune system, isn’t it?
In order to understand food sensitivities, we have to explore the concept of intestinal permeability. Indeed, the healthy intestinal membrane is exposed daily to numerous antigenic particles that are foreign to the human body. The intestinal membrane has specialized channels that enable it to absorb various nutrients and to discard anything else that it does not need: fiber, microbes, potentially pathogenic invaders, waste from food that is not absorbed etc. Just below the intestinal membrane lies a portion of the immune system called the GALT, the latter has important functions and acts as a gatekeeper (13) in case a pathogenic offender might escape previous mechanisms of defense and attempts to invade the body and access the general circulation. In case a parasite for example manages to invade and bypass the intestinal membrane, that invader will be attacked by macrophages or neutrophils and in case the attack is not successful, specific antibodies will be produced against the parasite and eventually he will be neutralized. Essentially the healthy intestinal membrane is impermeable to anything else than the right nutrients. (8)
Now let us look at what happens when the intestinal membrane stops being healthy or becomes an altered intestinal permeability site. (9)
Essentially the enterocytes, which are the cells that line the intestinal membrane, and which are normally bound by tight junctions, stop being tightly bound and start separating. The separation enables partially undigested food particles to penetrate the permeable gut lining and activate the GALT or immune system of the gut. The immune system then recognizes the partially digested food particles as "a foreign invader" and amounts an immune response to the food by producing IgG's. The antibodies further attack the food, as well as the already damaged intestinal membrane where the food binds, creating inflammation and damaging the villi, or specialized channels by which the food is absorbed. This inflammatory process further exacerbates the intestinal permeability and accelerates the rate at which new IgG's are produced to various foods. As a result, the affected individual starts developing food sensitivities as well as nutritional insufficiencies due to the altered ability to absorb nutrients. (10)
There are numerous risk factors that can lead to an altered intestinal permeability
Genetic susceptibility: some individuals especially those having a DAO SNP have a higher chance to develop food sensitivities and altered intestinal permeability (11)
Processed foods: A diet rich in these foods is also devoid of fiber, the latter being an important nutrient for the healthy microbiome. Processed foods also contain numerous food additives as well as trace pesticides and fungicides all of which can be inflammatory to the intestinal membrane (4)
Toxins: Exposure to environmental toxicants whether from a work exposure such as a farmer working in the field and spraying glyphosate on his crops or a factory worker involved in producing plastic components and exposed to BPA (6)
Nutritional insufficiencies: This 1 seems less apparent as a risk factor however not having enough vitamin D, vitamin A, or omega-3's can accelerate intestinal permeability if other risk factors are present
Chronic NSAIDs use: Ex: Advil or Naproxen. Anti-inflammatories can directly be damaging to the intestinal membrane, this is a well-known risk factor for gastrointestinal bleed especially in individuals over the age of 50.
Chronic alcohol Intake: Alcohol is a toxin to the gut and leads to inflammation and GI bleeds similarly to NSAIDS.
An intestinal infection such as a gastro caused by a virus or food intoxication caused by a bacterium such as Salmonella or a parasite infection such as that caused by Giardia or B Hominis. These gut infections can be a trigger for IBS by causing altered intestinal permeability (12)
Chronic Stress: High circulating levels of cortisol lead to generalized inflammation and can accelerate and cause altered intestinal permeability
Antibiotic use: Although life saving interventions in the right clinical context, antibiotics wipe out or deplete the healthy microbiome. This can cause gut dysbiosis and enhance local gut inflammation
Gut dysbiosis from eating processed foods for example, or from getting too many antibiotics (5)
High Athletic performance such as running a marathon. This causes a direct negative impact on the intestinal permeability for a short period of time
How do food sensitivities manifest clinically?
With local symptoms: This can look very much like IBS symptoms. Any combination of abdominal cramping, digestive upset, abnormal and inconsistent stool patterns, post-prandial bloating, reflux or excessive gas or belching. Also, people who manifest symptoms locally frequently tend to be more aware that they are suffering from food sensitivities and often can pinpoint an offending food and an exacerbation of one of their symptoms. Frequently these people have already tried changing their diet with variable success.
With Systemic symptoms: These can be broad and will vary from one individual to another. Symptoms can include but are not limited to:
- Fatigue
- Behavioural issues such as aggression or anxiety
- Headaches
- Brain fog or trouble thinking or concentrating
- Joint pains or stiffness
- Back pain
- Flushing or urticarial rash
- Eczema or Psoriasis
- Irritable Bladder
- Nose bleeds
- Hashimoto’s thyroiditis
- Etc
Individuals who experience systemic symptoms due to their food sensitivities may or may not experience local symptoms as well. In individuals who do not have local or gut symptoms, it is often harder to convince them to try an elimination diet and it takes them longer to see a clinical change after implementing such a diet because typically their pathology is more advanced. Indeed, when someone has reached the stage of experiencing systemic symptoms, they often have quite advanced intestinal permeability and gut dysbiosis. (15) (14) (5)
In my clinical experience I have found that food sensitivities are often an important contributing factor to many chronic diseases and chronic symptoms. Occasionally identifying and removing the offending foods feels nothing short of a miracle for the patient with daily migraines for example.
We have seen how local inflammation can drive local gut symptoms in the case of intestinal permeability but how can this become a systemic problem?
In fact, once the intestinal membrane stops functioning well as a barrier or a gatekeeper this leads to absorption of numerous antigenic particles. An antigen is simply something that can trigger the immune system. And many things can trigger the immune system: partially digested foods, beneficial microbes and pathogenic microbes and toxins are the most common offenders. Microbes also produce LPS or lipopolysaccharides which are highly inflammatory, and these compounds are also absorbed by the faulty barrier leading to systemic inflammation. LPS is often found in sepsis patients in high amounts, and this leads to such profound inflammation and immune activation in those patients that it can progress to septic shock and multiorgan failure. Therefore, it should come to no surprise that small systemic absorption of LPS should generate chronic inflammation. (17) (16)
The question I asked earlier in this blog was: can food sensitivities present with immediate symptoms, within minutes of exposure?
Yes, it can. Here is how:
The immune system of the gut is comprised of numerous cells, one of which is called the mast cell. This immune cell is typically involved in allergic symptoms. We can find mast cells in all mucous membranes and in all organs that have a communication with the external environment, or outside the body of the individual. Therefore, mast cells can be found in the nasopharynx, in the whole gastrointestinal tract, in the bladder, in the vagina and in the respiratory epithelium of the bronchial tree and lungs.
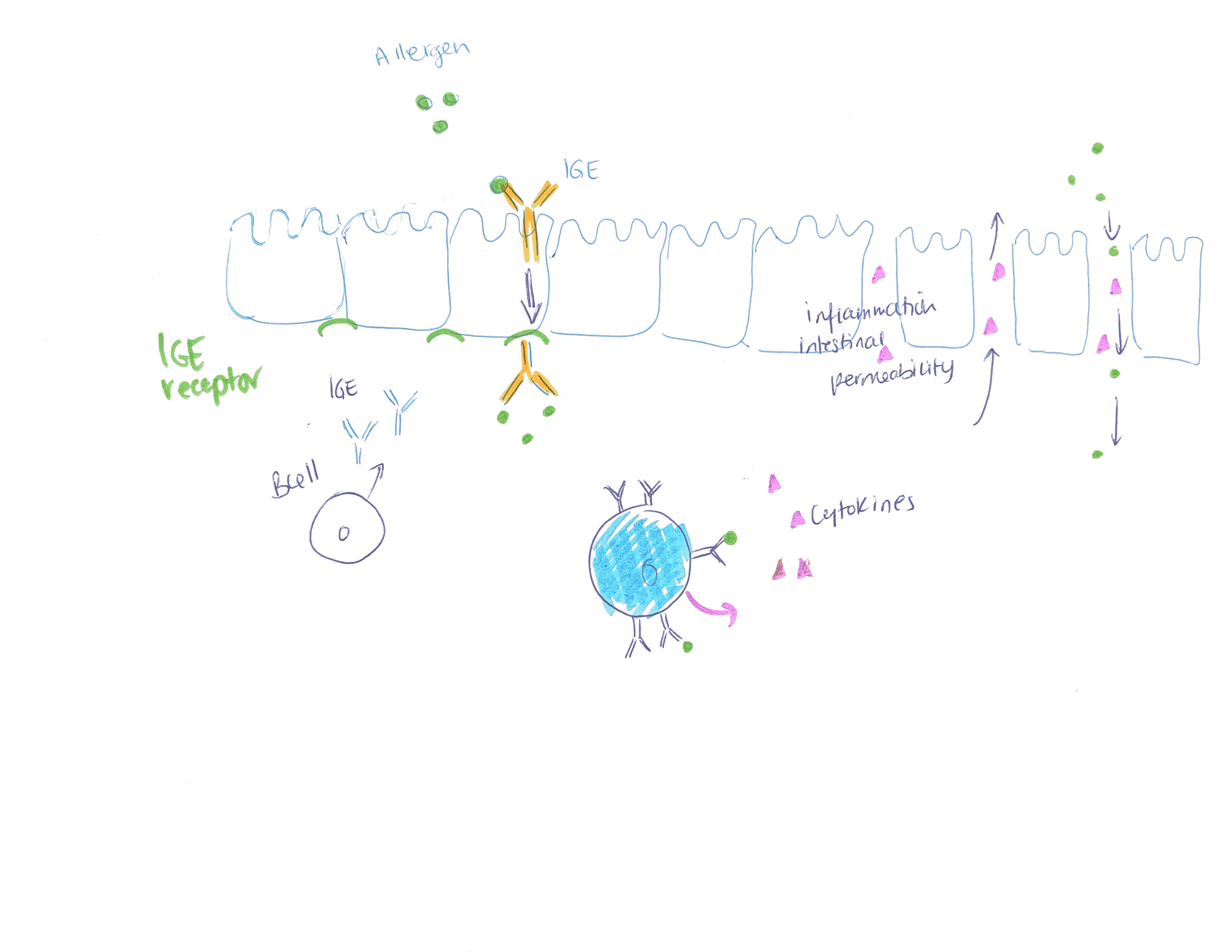
Mast cells typically lie dormant in the mucosal structure that lies on top of the intestinal cells. In a patient with other allergies such as environmental allergies, their immune system is more reactive than normal and tends to secrete more IGEs. The IGEs bind to the allergen and this new complex can activate dormant mast cells. Upon activation, mast cells release inflammatory cytokines and mediators locally and these further contribute to intestinal permeability and can generate immediate symptoms, as soon as the offending food touches the epithelial barrier. This then explains why certain patients suffering from food sensitivities can feel bad “RIGHT AWAY” as soon as they eat the wrong food. I caution practitioners to believe their patients when they have identified such reactions, they are very real. (18) (19)
How can food sensitivities be diagnosed?
There are tests on the market that evaluate IGG production to foods. One such test is carried by Great Plains Laboratories and another by Genova Diagnostics. They dose the IGGs and give a report that names all the foods tested as well as the level of reactivity to each food using a colour graded chart. Foods that react a lot are given a red colour and foods in green do not react typically. Then at the end of the report they include a suggestion of diet that removes the highest reactive foods.
These tests, in my opinion, have not yet reached prime time and for now have some limitations.
1- In the case of a patient suffering from advanced abnormal intestinal permeability and if that condition has been in development for years, typically the test will show most foods in the red category. The correct interpretation of such a finding would be to either test further or treat the intestinal permeability and consider repeat testing 3 months later for more accurate results
2- Different eating habits in the day or days prior to testing can cause falsely elevated IGGs to that food. Example someone who binges on pears the day prior to the test might show high reactivity to the test but in fact this is not a true positive result
3- The reproducibility of the test needs to be further improved. If the same person tests on three consecutive days there will be fluctuations in the results obtained. Typically, the foods in the red will be consistent or the same but foods in the yellow or green might change and this raises the question whether results are really reliable.
The gold standard for most functional medicine practitioners to this day remains the Elimination Diet (3)
This diet eliminates the foods that have the highest likelihood of being involved in a food sensitivity reaction from statistics taken on the general population. These diets can further be tailored to the individual patient as well as to their clinical situation. The foods that are restricted on the classical elimination diet are:
- Gluten
- Corn
- Soy
- Dairy
- Eggs
- Alcohol
- Coffee
- Sugar
- Preservatives and additives in food
- Nightshade vegetables: tomatoes, potatoes, peppers and eggplants
- Peanuts
This diet is typically followed for a minimum of 4 weeks and up to 12 weeks. The 4 weeks or 30 days comes from the fact that the half life of an IGG antibody is 30 days. Therefore, when a patient stops eating the offending foods for 30 days, then the number of antibodies they have at the end of the period is half the original amount. This lowers the reactions a person will have when re-introducing the foods omitted at the end of the diet period.
After the elimination diet, patients are encouraged to re-introduce foods (2) one at the time every 2-5 days and carefully monitor their symptoms during this time, as well as their food intake. If no symptoms occur during that period of re-introduction then the food is considered safe and re-introduced, otherwise it is omitted from the diet and will be re-introduced 3 months later to see if tolerated.
In addition to the elimination diet, in functional medicine we have tools to accelerate healing of the affected intestinal membrane in order to restore the original function of the gut lining which is selective absorption of nutrients.
Here are some supplements that can help with altered intestinal permeability
Turmeric : This potent anti-inflammatory acts on numerous receptors such as NFKB, LOX and COX to quench inflammation as well as accelerate healing through activation of NRF2 (20)
Vitamin D: this hormone is essential for the proper function of the innate immune system, it serves as an immunomodulator. It has important properties allowing for repair and healing of the gut membrane. In addition, this nutrient is frequently deficient or insufficient in the Northern Hemisphere
Vitamin A: Boosts NK cells which improves the function of the innate immune system, helps to raise secretory IGAs in the gut and accelerates healing and repair of the gut membrane
L-glutamine: this amino acid serves as fuel for the enterocytes allowing to rebuild them
Probiotics: they affect the gut microbiome and improving dysbiosis is another step forward in restoring a functioning GALT
Prebiotics: this feeds the healthy microbiome and therefore improves the intestinal milieu and helps to lower inflammation. This supplement can be omitted if the diet is rich in fiber (25-30 grams per day) (5)
Omega 3: This potent anti-inflammatory inhibits NFKB, inhibits arachidonic acid (major precursor for inflammatory cytokines) and stimulates production of resolvins (as their name implies they help resolve inflammatory reactions). Western diets are rich in Omega 6 oils which are pro-inflammatory. (21) (22)
These supplements, taken at the right doses by reputable supplement companies and given enough time to work (usually 3 months) can really accelerate improvement of IBS symptoms, improve food sensitivities and even allergic reactions mediated by mast cells. This works better when combined with the Elimination Diet. For doses and for customisation of this intestinal healing approach, please work with your health care provider since all these supplements might not be right for you. As always, I believe in informing the public of what they can do to take back control of their health.
This article is for educational purposes only and is not meant to be a replacement of a doctor-patient relationship.
References:
(2) Atkinson W and all. Food elimination based on IGG antibodies in irritable bowel syndrome: a randomised controlled trial Gut 2004; 53: 1459-1469
(3) Drisko J and all. Treating irritable bowel syndrome with a food elimination diet followed by food challenge and probiotics. J Am Coll Nutr 2006; 25: 514-522
(4) Roca-Saavedra P and all Food additivies, contaminants and other minor components: effects on human gut microbiota-a review. J Physiol Biochem. 2018 Feb; 74 (1): 69-83.
(5) Le Bastard Q and all. Systematic review: human gut dysbiosis induced by non antibiotic prescription medications. Aliment Pharmacol Ther. 2018 May; 126:454-467
(6) Jin y and al. Effects of environmental pollutants on gut microbiota. Environ Pollut. 2017 Mar; 222 :1-9
(7) Lomer MC Review article : the etiology, diagnosis, mechanisms and clinical evidence for food intolerance. Aliment Pharmacol 2015 Feb;41(3):262-75
(8) Turner JR Molecular Basis of Epithelial Barrier Regulation. The American Journal of Pathology. 2006;169(6):1901-1909
(9) Sartor RB and al Importance of intestinal mucosal immunity and luminal bacterial cell wall polymers in the etiology of inflammatory joint diseases. Baillieres Clinical Rheumatology. 1989;3(2):223-245
(10) Shi N and all Interaction between the gut microbiome and mucosal immune system. Mil Med Res. 2017; 4:14. Published 2017 Apr 27
(11) Xie, H, SH, “Roles of histamine and its receptors in allergic and inflammatory bowel diseases”, World Journal of Gastroenterology, 21 May 2005
(12) Parasitic infections in irritable bowel syndrome patients: evidence to propose a possible link, based on a case-control study in the south of Iran
(13) Brandtzaeg P And al Gate-keeper function of the intestinal epithelium. Benef Microbes. 2013 Mar 1;4(1):67-82
(14) Fasano A and al. Mechanisms of disease: the role of intestinal barrier function in the pathogenesis of gastrointestinal auto-immune diseases. Nat Clin Pract Gastroenterol Hepatol. 2005 Sep;2(9):416-22
(15) Brown and al. Diet induced dysbiosis of the intestinal microbiota and the effects on immunity and disease. Nutrients. 2012;4(8):1095-1119
(16) Arrieta MC and al Alterations in intestinal permeability. Gut 2006;55(10):1512-1520
(17) Riccio and al Undigested Food and Gut Microbiota may cooperate in the pathogenesis of Neuroinflammatory Diseases: a matter of barriers and proposal on the origin of organ specificity. Nutrient. 2019;11(11):2714 2019 Nov 9
(18) Yu LC and al. Intestinal epithelial barrier dysfunction in food hypersensitivity. J Allergy (Cairo) 2012;2012:596081 Sept 8 2011
(19) Perrier C and al Gut permeability and food allergies Clin Exp Allergy 2011 Jan;41(1):20-8
(20) Aggarwal and al 2005 Suppression of the nuclear factor KB activatoion pathway by spice derived phytochemicals: reasoning for seasoning. Annals of the New York Academy of Sciences. 1030. 434-41
(21) Jiang J and al Effect of Marine-Derived omega3 Polyunsaturated Fatty acids on Major Eicosanoids: a systematic Review and Meta Analysis from 18 Randomized controlled trials PLos One 2016;11(1):e0147351 Published 2016 Jan
(22) Williams-Bey and al Omega 3 free fatty acids suppress macrophage inflammasome activation by inhibiting NFKB activation and enhancing autophagy PLos One 2014 Jun 9;(6):e97957
